Metformin and gliclazide are two popular treatment options for type 2 diabetes. Metformin vs gliclazide is a review of key facts between both drugs.
Table of Contents
- Key terminology
- Metformin vs gliclazide: classification and mechanism of action
- How does metformin work?
- Role of metformin and gliclazide in the management of diabetes
- Metformin vs gliclazide: side effects
- What forms of metformin and gliclazide exist?
- Can metformin and gliclazide be taken together?
- Metformin vs gliclazide: which drug is more popular?
- Is metformin better than gliclazide?
- Conclusion
Key terminology
Glucose: a simple sugar which is used as an energy source by the body.
Insulin: a hormone produced in the pancreas. Insulin regulates the use of glucose in the body. In type 2 diabetes insulin
Type 2 diabetes: a condition characterised by a high level of sugar in the blood (body). Patients with type 2 diabetes do not produce sufficient amounts of insulin or the response to insulin in the body is negatively affected. This unables body to use glucose correctly and consequently increases the amount of sugar in the blood.
HbA1c: Glycated haemoglobin. Commonly, Hba1c is referred to as a blood test which shows average blood sugar levels over the last 2-3 months.
What is diabetes? (video)
Metformin vs gliclazide: classification and mechanism of action
Metformin and gliclazide are broadly classified as antidiabetic drugs. Both drugs are prescription-only medicines, which means patients need to get a prescription to get a supply of either of the drugs. Although metformin and gliclazide are used in the management of type 2 diabetes, both drugs have a distinct mechanism of action.
How does metformin work?
Metformin is the only biguanide type of drug available in the UK for the treatment of type 2 diabetes. Metformin has multiple modes of action (Rena et al., 2017). In simple terms, metformin reduces the production of glucose in the liver. Metformin has no impact on the release of insulin, as opposed to gliclazide. Additionally, metformin increases the use of glucose in insulin-sensitive tissues (Kefas et al., 2004).
Gliclazide is classified as a sulphonylurea drug. Gliclazide is one of few sulphonylurea drugs used in the treatment of type 2 diabetes in the UK. Gliclazide and other sulfonylureas increase insulin secretion. Gliclizde therefore can commonly cause hypoglycaemia (a low sugar level) as opposed to metformin which does not affect insulin release.
Role of metformin and gliclazide in the management of diabetes
The selection of the initial drug in the management of type 2 diabetes depends on different factors. Metformin is seen as a ‘gold standard’ in the management of diabetes and is commonly chosen as a first-line treatment. Gliclazide may however be considered as first-line treatment in diabetic patients who have high sugar levels with associated symptoms. (NICE, 2022) Further down the recommended pathway gliclazide is one of the options of dual therapy with metformin.
Metformin vs gliclazide: side effects
Taking any medication comes with a risk of possible side effects. The table below lists possible,
common side effects for metformin and gliclazide (BNF, 2022).
|
Metformin vs gliclazide: common side effects |
|
|
Metformin |
Gliclazide |
| Abdominal pain
Diarrhoea, Vomiting, Taste disturbance, Appetite decreased |
Abdominal pain
Diarrhoea Nausea Hypoglycaemia (low sugar level) |
Gastrointestinal side effects caused by metformin are most common at the beginning of the treatment and some of them are transient. Side effects may be persistent in some patients, especially those treated with a higher dose of metformin. Patients who find metformin’s side effect troublesome may ask their doctor to consider prescribing a modified-release (slow release) form of metformin, which is associated with lesser amounts of gastrointestinal side effects.
Some gastrointestinal side effects which may be experienced when taking gliclazide are similar to those of metformin. Gliclazide may cause hypoglycaemia (low sugar level), which is not possible with metformin. The risk of hypoglycaemia with gliclazide and not metformin highlights the difference in mechanism of action between both drugs.
What forms of metformin and gliclazide exist?
Gliclazide comes only in two forms: tablet and modified-release tablets of various strengths. Metformin on the other side comes as:
- Tablets
- Modified -release tablets
- Oral solution and
- Powder
Can metformin and gliclazide be taken together?
Treatment of type 2 diabetes in patients whose condition does not improve is managed in a stepwise manner, which means treatment with two or more antidiabetic drugs. For example, patients who fail to control HbA1c with one drug, like metformin, may be offered a second drug, which may belong to the following class of antidiabetic drugs(NICE, 2022):
- a DPP‑4 inhibitor or
- pioglitazone or
- a sulfonylurea (gliclazide) or
- an SGLT2 inhibitor
Patients therefore may be treated with metformin and gliclazide at the same time. Metformin and gliclazide can be taken together. Taking gliclazide and metformin may increase the risk of hypoglycaemia (low sugar level).
Metformin vs gliclazide: which drug is more popular?
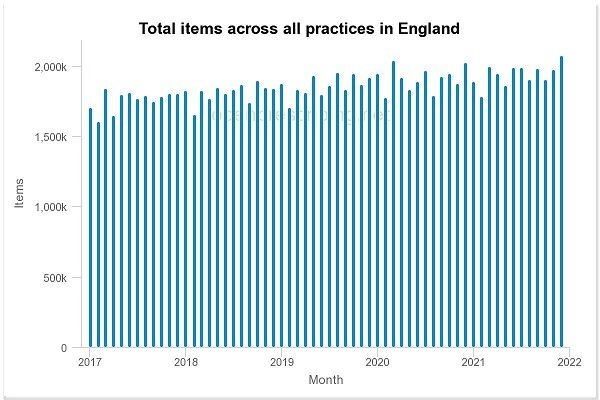
Prescribing statistics in England clearly show that metformin is a more popular drug than gliclazide with over 23.3 mln prescriptions issued in 2021. 6.3 mln prescriptions were issued for gliclazide in 2021.
When looking at the trend for prescribing, the number of prescriptions issued for gliclazide is decreasing, whereas for metformin are increasing.

Is metformin better than gliclazide?
Two key areas which may help to answer the above question are the safety of the drug (possible side effects) and efficacy (reduction of HbA1c). When used alone, metformin and gliclazide have a similar estimated effect on the reduction of HbA1c which stands at 1-2% (Chaudhury et al., 2017.
The addition of gliclazide to metformin, or any other antidiabetic from different classes improves glucose control (Qian et al., 2018). The risk of hypoglycaemia increases significantly when gliclazide is taken with another antidiabetic drug (Qian et al., 2018).
Metformin is not associated with the risk of hypoglycaemia, and overall has a better safety profile than gliclazide. As studies have shown, gliclazide may increase weight gain, an important factor that needs consideration when the treatment of diabetes is considered.
Perhaps the risk of hypoglycaemia and the possibility of weight gain drives the downturn in gliclazide prescribing.
Conclusion
Metformin became one of the most prescribed (overall) medicines in England. Despite the lack of clear evidence for better efficacy in HbA1c reduction when compared to gliclazide, metformin became the preferable treatment choice in patients with type 2 diabetes with a better safety profile than gliclazide.
Lifestyle changes, physical exercise and a healthy diet for example play important, not only delaying the development of diabetes in pre-diabetic patients but also improving control of sugar (glycemic control) with reduction of HbA1C levels (Chaudhury et al., 2017).
References:
BNF, British National Formulary (2022). Gliclazide: side effects. Available at: https://bnf.nice.org.uk/drug/gliclazide.html#sideEffects Accessed on 23/03/2022
BNF, British National Formulary (2022). Metformin: side effects. Available at: https://bnf.nice.org.uk/drug/metformin-hydrochloride.html#sideEffects Accessed on 23/03/2022
Chaudhury A, Duvoor C, Reddy Dendi VS, Kraleti S, Chada A, Ravilla R, Marco A, Shekhawat NS, Montales MT, Kuriakose K, Sasapu A, Beebe A, Patil N, Musham CK, Lohani GP, Mirza W. Clinical Review of Antidiabetic Drugs: Implications for Type 2 Diabetes Mellitus Management. Front Endocrinol (Lausanne). 2017 Jan 24;8:6. doi: 10.3389/fendo.2017.00006. PMID: 28167928; PMCID: PMC5256065. Available at: https://dx.doi.org/10.3389%2Ffendo.2017.00006 Accessed on 23/03/2022
Kefas BA, Cai Y, Kerckhofs K, Ling Z, Martens G, Heimberg H, Pipeleers D, Van de Casteele M (2004). Metformin-induced stimulation of AMP-activated protein kinase in beta-cells impairs their glucose responsiveness and can lead to apoptosis. Biochem Pharmacol. 2004 Aug 1;68(3):409-16. doi: 10.1016/j.bcp.2004.04.003. PMID: 15242807. Available at: https://doi.org/10.1016/j.bcp.2004.04.003 Accessed on 21/03/2022
NICE (2022). Diabetes – type 2: Scenario: Management – adults. Available at: https://cks.nice.org.uk/topics/diabetes-type-2/management/management-adults/ Accessed on 23/03/2022
Qian D, Zhang T, Zheng P, Liang Z, Wang S, Xie J, Zhao L, Zhang Y, Situ B (2018). Comparison of Oral Antidiabetic Drugs as Add-On Treatments in Patients with Type 2 Diabetes Uncontrolled on Metformin: A Network Meta-Analysis. Diabetes Ther. 2018 Oct;9(5):1945-1958. doi: 10.1007/s13300-018-0482-5. Epub 2018 Aug 18. PMID: 30121726; PMCID: PMC6167280. Available at: https://doi.org/10.1007/s13300-018-0482-5 Accessed on 23/03/2022
Qian D, Zhang T, Tan X, Zheng P, Liang Z, Xie J, Jiang J, Situ B. Comparison of antidiabetic drugs added to sulfonylurea monotherapy in patients with type 2 diabetes mellitus: A network meta-analysis. PALoS One. 2018 Aug 27;13(8):e0202563. doi: 10.1371/journal.pone.0202563. PMID: 30148851; PMCID: PMC6110472. Available at: https://doi.org/10.1371/journal.pone.0202563 Accessed on 23/03/2022
Rena G, Hardie DG, Pearson ER (2017). The mechanisms of action of metformin. Diabetologia. 2017 Sep;60(9):1577-1585. doi: 10.1007/s00125-017-4342-z. Epub 2017 Aug 3. PMID: 28776086; PMCID: PMC5552828. Available at: https://doi.org/10.1007/s00125-017-4342-z Accessed on 21/032022





